
John Cumbers, Contributor
Dec. 9, 2020
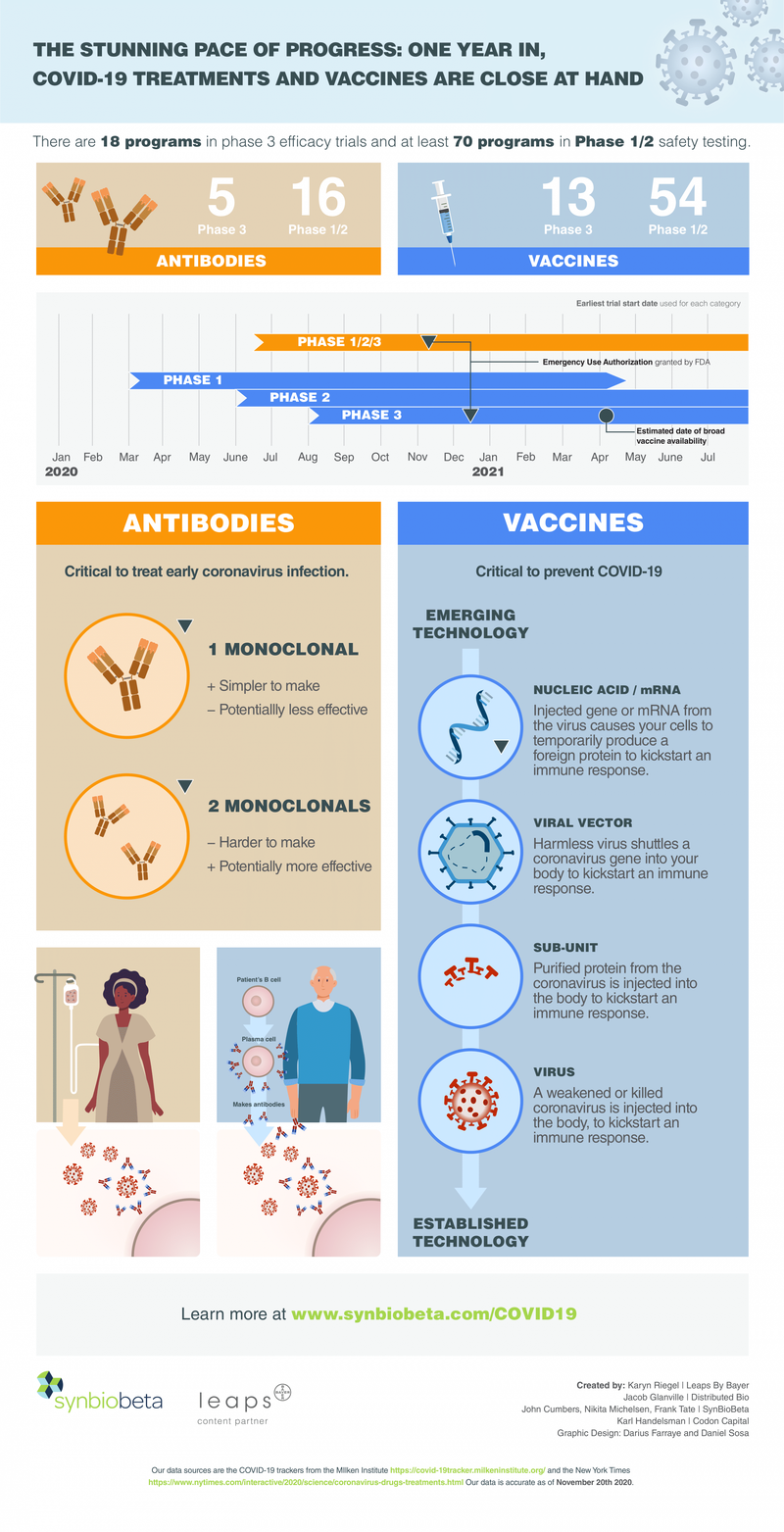
Since bursting onto the scene over a year ago, the COVID-19 pandemic has so far claimed well over one million lives. The ferocious spread of the virus first witnessed in the spring is now being dwarfed by an even larger surge, with hospitalizations at record highs. More deaths will inevitably follow. Yet despite this grim reality, hope has emerged.

Medical science is progressing faster than even the optimists had expected. So far, two of the most innovative COVID-19 vaccine candidates have reported efficacy over 95 percent, and a third with slightly lower efficacy but no need for freezer storage was just announced, making future distribution easier. Other newfound medical interventions have also more than halved the death rate from the virus.
Antibodies — whether spurred by a vaccine or directly injected — remain our best hope for ending the pandemic. Those who survive COVID-19 produce these virus-halting proteins in the process. For everyone else still living in fear, alternative ways of acquiring antibodies may be essential. Luckily, there are two ways to get them. One is to have antibodies directly injected into you, which may confer temporary immunity to or even treat infection if it hasn’t progressed very far. The other way is vaccination, which turns the body into its own antibody factory.
The global race to deliver proven antibody treatments and vaccines for COVID-19 is well underway. A slew of candidates — including many made possible by advances in synthetic biology — are in late-stage clinical trials. Beyond positive vaccine news, two antibody treatments by Eli Lilly and Regeneron were recently granted limited approval as treatment for COVID-19.
In March, I partnered with Leaps by Bayer, the impact investment arm of Bayer to create a visual overview of the race to develop treatments and vaccines against COVID-19. “It has been a year of blindingly fast scientific progress in a year that felt like a decade of social and economic stress.” said Jürg Eckhardt, Head of Leaps by Bayer. Here is an updated version showing where that race stands today.
The False Hope of Drug Reuse
Back in March, many scientists explored whether already-approved drugs could be reused to treat COVID, as this could deliver results quickly. Unfortunately, few of these bets paid off. The scientific method, however, did prevail. Hydroxychloroquine, the antimalarial drug touted by some as a COVID-19 remedy, did not show any benefit after a double-blinded placebo-controlled trial. In these trials, half the population receives the real drug, and the other half receives a placebo, a drug designed to appear like the real thing. Both groups are blind as to which version they are receiving and the researchers administering the experiments also don’t know, to prevent any biases from those giving the drug.
“We wasted a huge amount of public discourse on hydroxychloroquine, when the real story was scientists collaborating to quickly invent over a hundred vaccine and an additional one hundred antibody projects against Covid,” said Karl Handelsman, a biotech investor with San Francisco investment fund Codon Capital.
Remdesivir, an Ebola-fighting drug that did win FDA approval for coronavirus, was recently slammed by the World Health Organization to have no meaningful effect on COVID-19.
Dexamethasone, an anti-inflammatory steroid that was also seen as a hopeful candidate, has not shown positive results from careful trials.
And then there are treatments without any kind of scientific basis. Housing and Urban Development Secretary Ben Carson, a former neuroscientist, took the herbal supplement oleander extract being touted by Mike Lindell who served as President Trump's Minnesota campaign chair. Carson’s condition then became serious and he was also admitted to Walter Reed Medical Center to take the same antibody treatment that president Trump had received. "You know, what happened with Mike Lindell, who is a fantastic salesperson, but not a scientist, perhaps distorts the process," Carson said at the time.
“Repurposing sounded like a short cut. But people starting from scratch made antibodies and vaccines that were directly designed to target the virus showed efficacy in less than a year,” said Handelsman.
Antibody Treatments: The President’s Cocktail
Among antibody treatments that directly target the virus, two have won approval. One developed by New York-based Regeneron Pharmaceuticals received global attention when it was infused into President Trump following his COVID-19 diagnosis. Although he appears to have beaten back his infection, no one knows for sure whether the antibody treatment actually helped as the president was at the same time also receiving other experimental drugs.
The Regeneron product, called REGN-COV2, is a mixture or “cocktail” of two different monoclonal antibodies, both of which target proteins on the surface of the virus. They were discovered early in the year using Regeneron’s VelocImmune technology, which allows researchers to quickly identify human-like antibodies in mice.
To make the drug, both antibodies in the cocktail must be grown inside cells, extracted, and then mixed together to form the final product. This manufacturing detail matters as separate supply lines are needed for each protein component. Global capacity for making antibodies was already limited before the pandemic. Some factories are now dialing down production of other antibody drugs in order to free up capacity for COVID-19 treatments.
To further complicate matters, high doses of the Regeneron cocktail may be needed. President Trump was infused with a whopping eight grams of REGN-COV2. If much smaller doses prove ineffective, the world’s finite supply and limited manufacturing capacity will not stretch far. Operation Warp Speed, launched in April by the White House to hasten COVID-19 vaccines and treatments, has poured millions of dollars into boosting factory capacity for coronavirus antibody drugs.
In October, Regeneron filed for Emergency Use Authorization (EUA) with regulators in the United States. In November, REGN-COV2 was approved for limited use. An earlier trial involving hospitalized patients was halted, however, due to a possible safety concern with the drug.
Antibody Treatments: A Simpler Option?
An EUA was also granted in November for a different antibody drug. LY-CoV555, which is still in Phase 3 testing, was discovered by Vancouver-based AbCellera Biologics and developed by American pharmaceutical giant Eli Lilly. Unlike Regeneron’s cocktail, this treatment contains just one active antibody ingredient. It may therefore become the cheaper and more available option.
But treatments based on just one antibody must do more with less. Unfortunately, it appears LY-CoV555 alone cannot treat the sickest COVID-19 patients. In October, the National Institutes of Health, which oversees clinical testing of the drug, put a stop to trials involving hospitalized patients after initial findings revealed “a low likelihood that the intervention would be of clinical value” for that population.
In March, we projected the arrival of the first approved antibody treatments at the end of September. They arrived in November, but having two win limited approval before the year’s end reveals just how quickly modern tools for antibody discovery can produce life-saving treatments.
Vaccines: Establishing Safety
We also projected in the spring a standard path for COVID-19 vaccine trials: Phase 1 safety testing in a small, healthy group followed by Phase 2 safety testing in an expanded cohort followed by massive Phase 3 efficacy trials. In these extraordinary times however, regulators green lit an alternative approach: for several vaccine candidates, Phase 2 testing began before Phase 1 was complete. And some Phase 3 trials commenced before any Phase 2 trials had finished. This tiled approach — where one phase of a trail overlaps the end of another — still allows for the same amount of safety and efficacy date to be collected over time, but at a much accelerated pace. In the midst of a global pandemic, each month shaved from the testing timeline could save thousands of lives.
Luckily, no phase of any COVID-19 vaccine trial has had to end because of safety issues, though some have paused temporarily to investigate health scares. In September, AstraZeneca paused its Phase 3 vaccine trial to investigate a rare form of inflammation that appeared in one healthy volunteer. Following an investigation, regulators allowed the trial to resume. In October, Johnson & Johnson paused its Phase 3 vaccine trial over a single “unexplained illness,” resuming the trial eleven days later after a safety review.
Such pauses are common in late-stage clinical trials. Among any large group of people, random illness is bound to pop up, and Phase 3 vaccine trials, which can include tens of thousands of volunteers, are no exception. Safety pauses can even be interpreted as a good thing as they reveal that scrupulous safety monitoring of the clinical trials volunteers is indeed underway.
Vaccines: Four types vying for approval
All vaccines try to train the body to guard against an invader. Many coax the body into making its own protective antibodies, but how they accomplish this can vary. The race for COVID-19 vaccines is pitting new strategies against older, more established ones, with scientists hoping to maximize their chances of success.
Here are the most promising vaccines currently in Phase 3 testing, sorted by vaccine type.
1. NUCLEIC ACID VACCINES
Nucleic acid vaccines contain short gene segments —either RNA or DNA — which can temporarily cause your cells to produce foreign proteins. For COVID-19, it appears that inoculation with RNA molecules encoding a protein from the coronavirus is sufficient to kickstart immunity. Pfizer announced recently that its RNA vaccine candidate for COVID-19, developed in partnership with the German firm BioNTech, is more than 95 percent effective. This claim is based on initial data from a large Phase 3 trial. Moderna, which is also testing an mRNA vaccine for COVID-19, reported 94.5% efficacy from its interim Phase 3 results. “These stunning positive results were delivered by a new approach with the fastest path from identified pathogen to clinical trial. A speed which I hope can now be replicated again in the future” said Handelsman.
2. VIRAL VECTOR VACCINES
Rather than injecting RNA directly, the AstraZeneca/Oxford and Johnson & Johnson vaccines both rely on weakened cold virus to shuttle coronavirus genes into the body in order to spur an immune response. This virus-as-ferry technology is relatively new and largely unproven. Though both candidates remain promising, only one vaccine has ever been fully approved based on similar technology. That vaccine, made by the Chinese firm CanSino, is for Ebola. CanSino, as well as the Gamaleya Research Institute in Russia, are also trialing viral vector vaccines for COVID-19.
Early Phase 3 results from the AstraZeneca/Oxford vaccine appear to show 70% efficacy. A potential advantage of this vaccine is its stability — it does not need to be stored at very cold temperatures, making it much easier to distribute.
3. SUBUNIT VACCINES
A more conventional route to vaccination is to inject proteins or other non-genetic “subunits” from a pathogen. This has led to successful vaccines for whooping cough, anthrax, and cervical cancer. At the moment, only one company — Novavax, based in Gaithersburg, MD— has a subunit vaccine in Phase 3 testing. That vaccine contains the coronavirus spike protein arrayed onto a recombinant protein nanoparticle.
4. VIRUS VACCINES
Finally, the most established method for achieving vaccine-induced immunity is to inoculate with a weakened or killed virus directly. This method has produced successful vaccinations for polio vaccine, hepatitis A, and rabies. At present, Sinovac, Bharat Biotech based in India, and the Murdoch Children’s Research Institute in Australia are pursuing virus-based vaccines for COVID-19.
A race with multiple winners
In the end, several vaccines that use different technologies will likely prove successful. This outcome would be good news for all. With more vaccine options, there will be more supply and more lives saved. Similarly, additional antibody treatments for stopping the virus as well some that counteract the immune overreaction which characterizes severe COVID-19 are likely to emerge in the coming months.
We are living through a remarkable moment in science, where it is easier than ever to build life-saving compounds using biology. That at least is something to feel good about.
John Cumbers, Contributor
© 2024 Forbes Media LLC. All Rights Reserved
This Forbes article was legally licensed through AdvisorStream.


